While many have lamented the social and economic impacts of the COVID-19 pandemic, for 21 million Americans, it offered consistent access to healthcare that many didn’t have before.
Under the 2020 Coronavirus Aid, Relief, and Economic Security Act (CARES Act) states could not remove anyone from Medicaid – the program that offers health insurance to the poorest in the U.S. – even if they suddenly couldn’t qualify for it.
States also couldn’t dis-enroll anyone from the Children’s Health Insurance Program (CHIP), which provides healthcare to kids and their caregivers who make too much to qualify for Medicaid, but can’t afford private insurance.
The point was to prevent anyone from losing access to healthcare during a public health emergency.
And it worked.
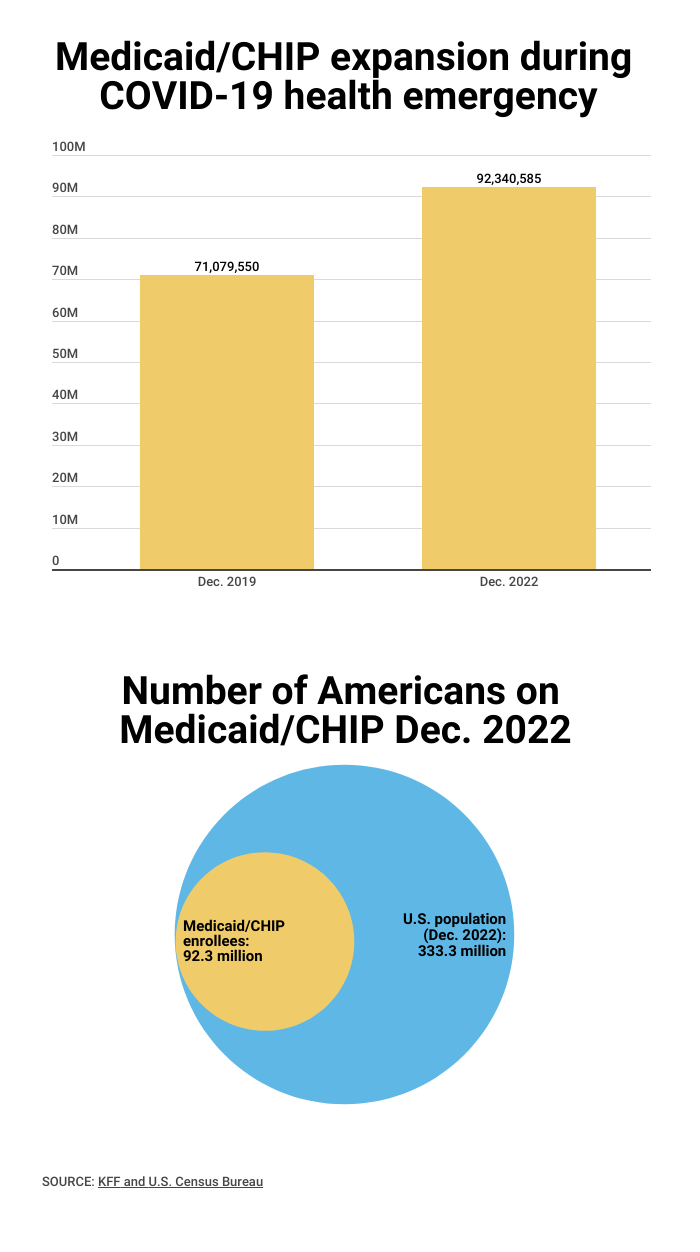
Medicaid and CHIP currently cover 92 million people, a 30 percent increase from 71 million before the pandemic. By 2022, the uninsured rate was only 8 percent - the lowest it’s been in U.S. history.
But this will all soon change as Congress allowed the stop gap measure to begin phasing out on April 1 – a month before the COVID emergency is set to expire – in a 14-month process the government calls “unwinding”.
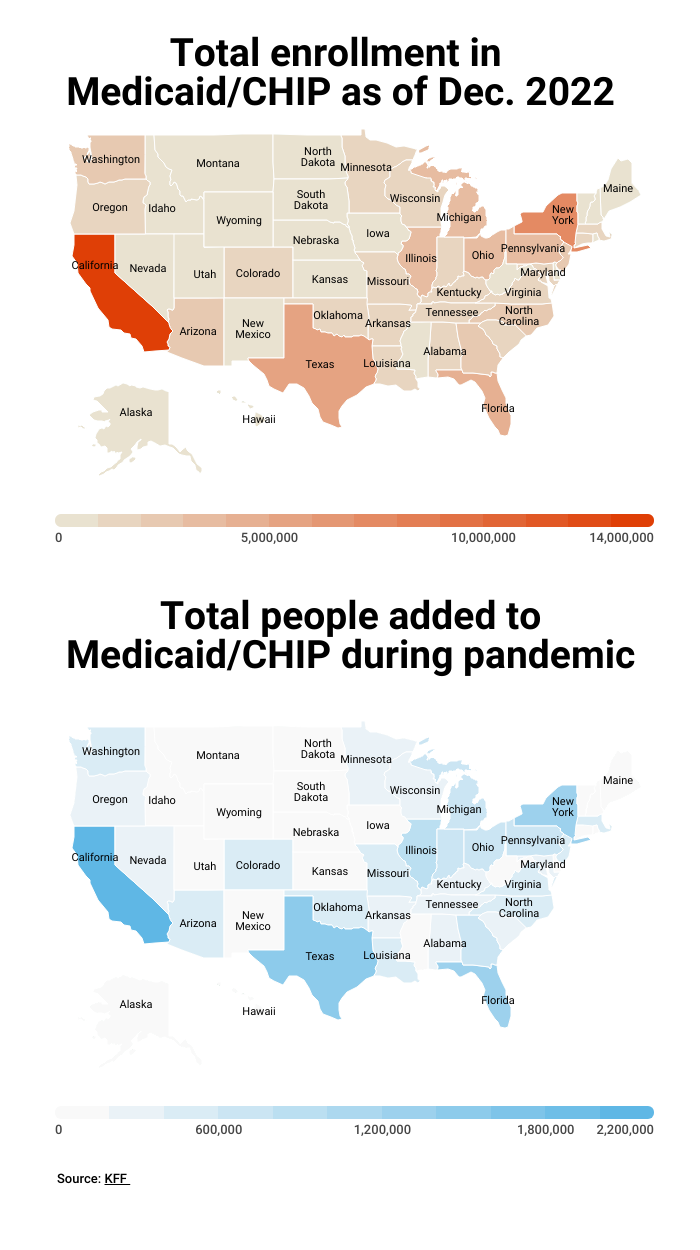
The Dept. of Health and Human Services projects that about 15 million people, including children, will be dis-enrolled from Medicaid and CHIP in this process. About 7 million of them are estimated to be people who are still eligible for coverage.
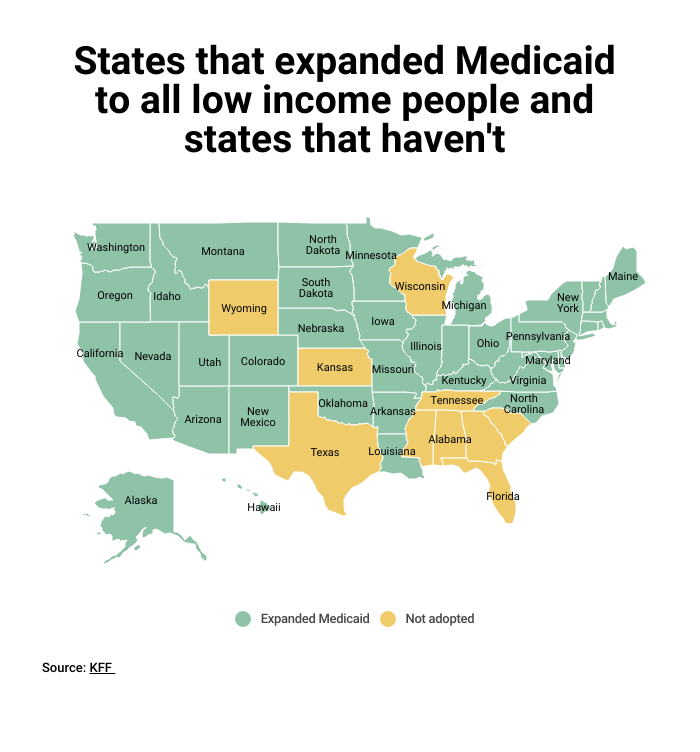
In states that approved expanded Medicaid under the 2010 Affordable Care Act, low-income Americans with income up to 138 percent of the federal poverty level can still receive healthcare as long as they meet the deadlines to re-enroll. (See the deadlines for each state)
But for the 20 million people currently enrolled in Medicaid and CHIP in Texas, Florida, Georgia, Wisconsin, Tennessee, South Carolina, Alabama, Mississippi, Kansas, and Wyoming – ten states that have foregone federal funding to expand Medicaid to their state’s poorest – access to healthcare is at risk.
It’s estimated that 1.9 million people would no longer have medical coverage in these states, and about 76 percent of them will be childless adults, KFF reports.
MOST VULNERABLE ARE MOST AFFECTED
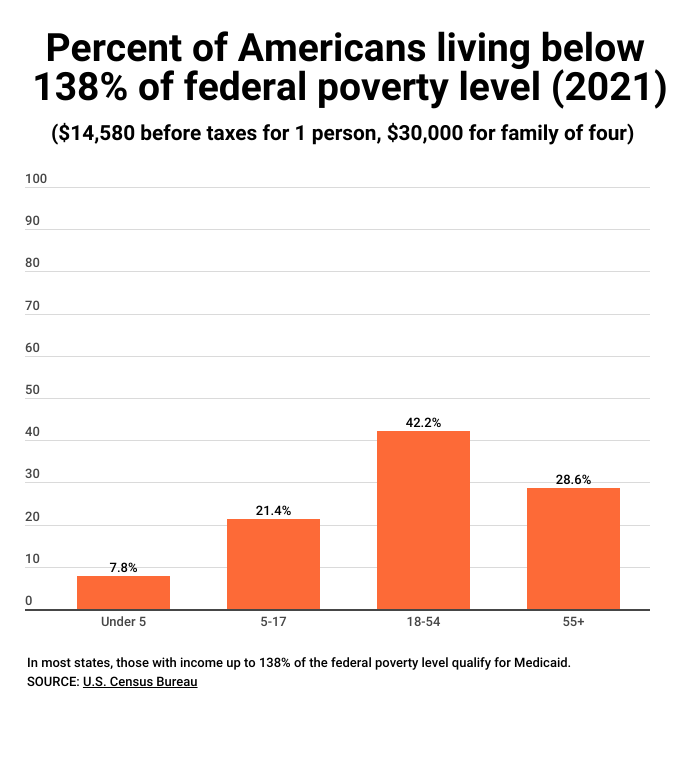
When it passed in 2010, the Affordable Care Act increased the income limits to qualify for free medical care for non-elderly adults up to 138 percent of the federal poverty level. The federal poverty level is currently $14,580 for one person. In return, states would get matching federal funds, which is currently at 90 percent.
Since the Supreme Court ruled in 2012 that expanded Medicaid was optional to states, in the ten states that have not expanded the program, Medicaid is only available to families who make, on median, below 38 percent of the federal poverty level. That would amount to $9,447 for a family of three, KFF reports.
In all non-expansion states, except Wisconsin, adults without children are not eligible for Medicaid at all, regardless of income.
Other findings from KFF:
In Texas, which has the strictest income requirements for Medicaid, parents in a family of three that make more than $3,977 a year are not eligible for Medicaid.
Families that earn below the federal poverty level, but above their state’s eligibility for Medicaid also do not qualify for subsidies in the healthcare marketplace.
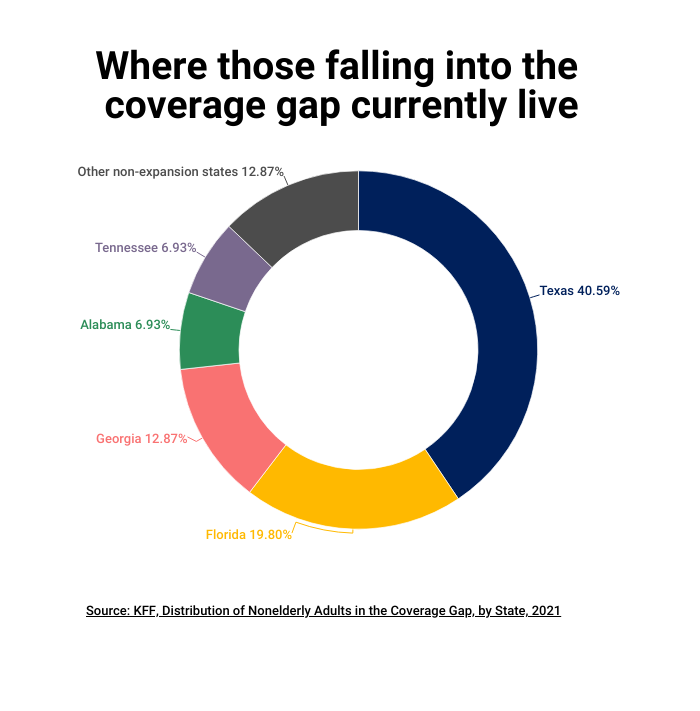
Adults losing coverage in non-expansion states will primarily be in three Southern states: Texas, Florida and Georgia.
More than 60 percent of the adults in the coverage gap are people of color.
Sixty percent of people in the coverage gap are in a family with a person who is employed, and 50 percent are working themselves, in low paying jobs.
The most common jobs for people losing coverage are: cashier, cook, waiter/waitress, construction laborer, maid/housecleaner, retail sales, and janitor.
Fifteen percent of people in the coverage gap have a disability such as serious difficulty in hearing, vision, cognitive functions, mobility and independent living.
People between the ages of 55-64 make up 17 percent of those in the coverage gap. Many will leave their health needs untreated until they are eligible for Medicare at 65.
For more, check out our exclusive content on CGTN Now and subscribe to our weekly newsletter, The China Report.